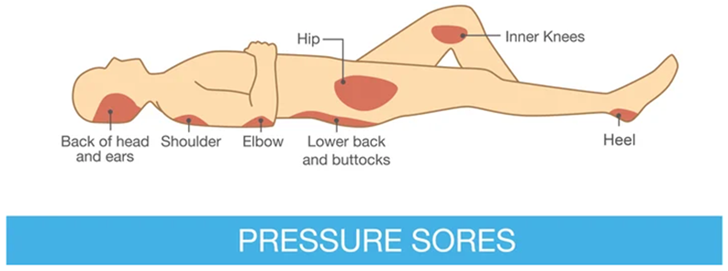
Bedsores, also called pressure ulcers or pressure injuries , are a serious concern for individuals who are confined to a bed or wheelchair for extended periods. They occur when sustained pressure on an area of skin cuts off blood circulation, leading to tissue damage and the formation of open wounds. This is especially significant for those who cannot reposition themselves regularly.
Bedsores can start as innocuous-looking red areas, but they can quickly progress to deeper wounds causing pain, infection, and in severe cases, lead to life-threatening complications.
In this awareness guide, we will share cited resources to learn more about preventing pressure injuries and some helpful options to consider to improve quality of care.
1. Frequent Repositioning
According to medlineplus.gov, changing the person's position every two hours is crucial. It relieves pressure on vulnerable areas like the heels, hips, tailbone, and shoulder blades.
John Hopkins Medicine recommends that If the person is confined to a wheelchair, encourage shifts in position every 15 minutes.
2. Specialized Beds & Support Surfaces
Some individuals require specialized mattresses, overlays, and cushions designed to redistribute pressure. These may include foam, air-filled, or gel-based surfaces. While these solutions are a great starting point, they are often insufficient for long-term pressure injury reduction.
Medical beds featuring lateral rotation technology can dramatically reduce the risk of pressure injuries. These beds gently and periodically turn the patient from side to side, continuously changing their pressure points, improving blood flow, and reducing sleep disturbances.
3. Skincare and Hygiene
Skincare plays a crucial role in preventing bedsores . Here are key aspects to be aware of and ask your physician about:
Cleanliness: Maintaining clean and dry skin, particularly in areas vulnerable to pressure ulcers, is vital. Use mild, gentle cleansers and avoid excessive moisture.
Hydration: While essential, over-moisturization can also be a concern. Seek guidance on suitable moisturizers and their appropriate application.
Friction reduction: Reduce instances of friction with furniture and essential items. Discuss your patient's individual situation with a healthcare provider.

4. Proper Nutrition and Hydration
Eating a balanced diet and staying adequately hydrated promote skin health and healing. Consider a protein-rich diet, vitamins, and minerals.
Consult a dietician for guidance on providing a well-rounded diet suitable for the person's need and health condition. It is important to be aware of these areas and how they play a long-term role in reducing complications.
5. Regular Skin Inspections
Carefully examine the patient's skin daily, particularly over bony areas. Look for:
-
Changes in skin color (redness, darkness, paleness)
-
Warm or cool patches compared to surrounding skin
-
Swelling or firmness
-
Blisters or open wounds
You should always consult a physician before taking your own remediative actions and be sure to learn about the stages of symptoms to watch out for.
6. Addressing Other Risk Factors
Reduce Shear and Friction: Assist the person when repositioning to prevent skin dragging that can result in tissue tears. Use draw sheets for transfers and repositioning.
Manage Underlying Medical Conditions: Conditions like diabetes and circulation issues can worsen pressure injury risk, so ensure these are appropriately managed.
7. Consult a Healthcare Professional
If a bedsore develops, immediately start work with a doctor or wound care specialist for a treatment plan that may involve cleaning, dressing, and in more severe cases, other interventions.
Prevention is Key
The best way to manage bedsores is to prevent them from happening in the first place. These proactive measures offer the best chance to maintain the patient's health, comfort, and quality of life.
In addition to the immediate health benefits, the reduced risk of increasing medical expenses is a major bonus that cannot be overstated.
Sources:
Medline Plus: Bedsores
[https://medlineplus.gov/ency/patientinstructions/000426.htm]
Johns Hopkins Medicine: Bedsores
[https://www.hopkinsmedicine.org/health/conditions-and-diseases/bedsores]
Cleveland Clinic: Bedsores (Pressure Ulcers)
[https://my.clevelandclinic.org/health/diseases/17823-bedsores-pressure-injuries]
National Library of Medicine (NIH): Preventing pressure ulcers
[https://www.ncbi.nlm.nih.gov/books/NBK326430/]
Disclaimer: This article provides general information on bedsore prevention from cited sources, please consult with healthcare professionals for recommendations appropriate to your patient's specific circumstances.

